Overview of the Tuskegee Syphilis Study
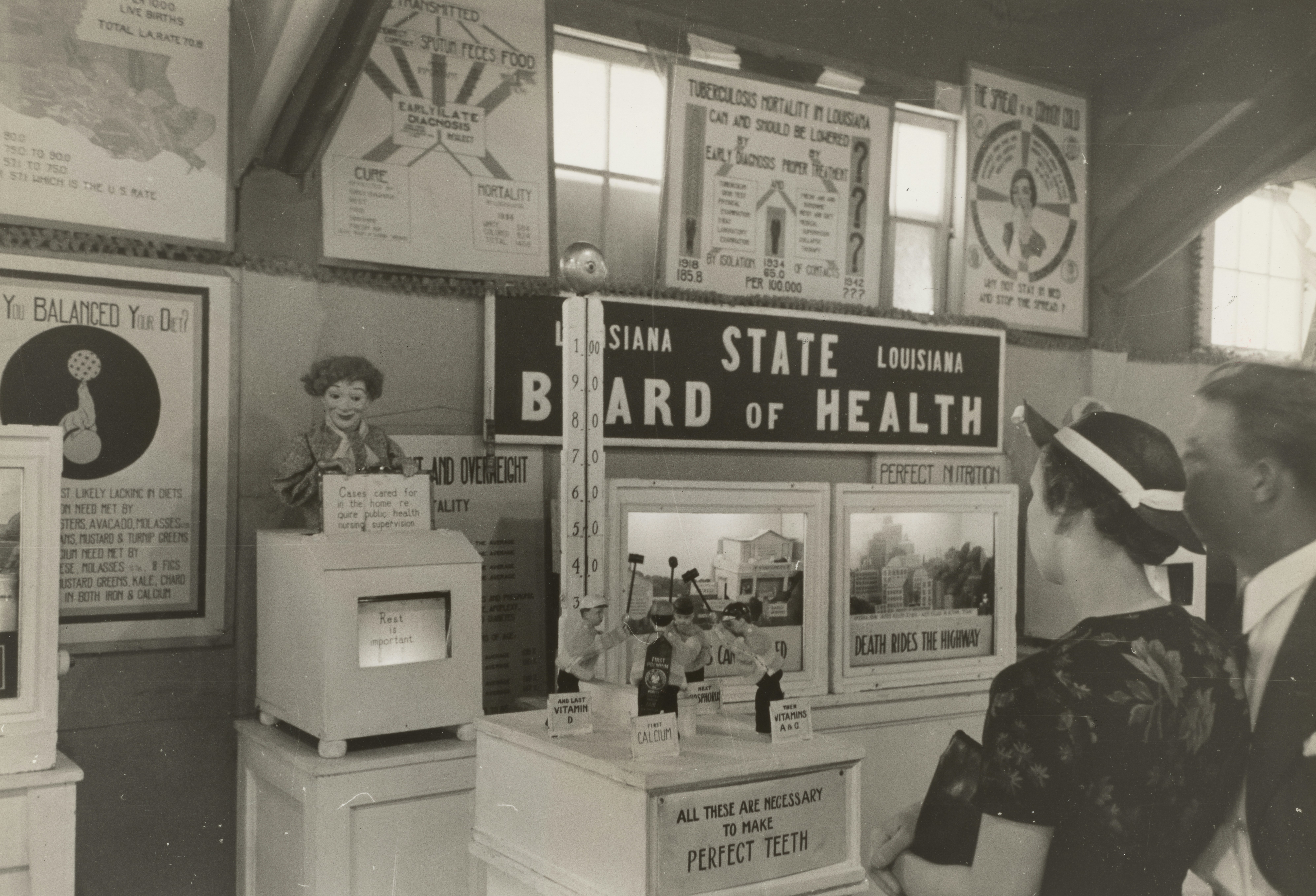
The Tuskegee Syphilis Study, conducted from 1932 to 1972, represents a significant and disturbing period in the history of medical ethics. This research project was initiated by the U.S. Public Health Service with the primary objective of observing the natural progression of untreated syphilis in African American men. The study took place in Macon County, Alabama, and involved 399 men diagnosed with syphilis, alongside a control group of 201 subjects who were not infected.
At the inception of the study, the men were not informed of their diagnosis nor the true purpose of the research. Instead, they were told that they were receiving free healthcare from the government for “bad blood,” which was a term used to describe a variety of ailments. The participants were misled about the treatment process, as they were denied access to penicillin, the proven effective treatment for syphilis, which became widely available in the 1940s. This decision was rooted in the study’s controversial aim, which was to collect and analyze data on the effects of the disease over time without providing necessary medical intervention.
The ethical concerns surrounding the Tuskegee Syphilis Study are glaring. Not only did the researchers fail to obtain informed consent from the participants, but they also exploited a vulnerable population who had limited access to healthcare and education. This lack of transparency and respect for the men’s autonomy has led to significant criticism of the study, resulting in a profound erosion of trust in medical institutions among African American communities, which persists to this day. Ultimately, the Tuskegee Syphilis Study serves as a cautionary tale about the importance of ethical standards and the necessity of informed consent in medical research.
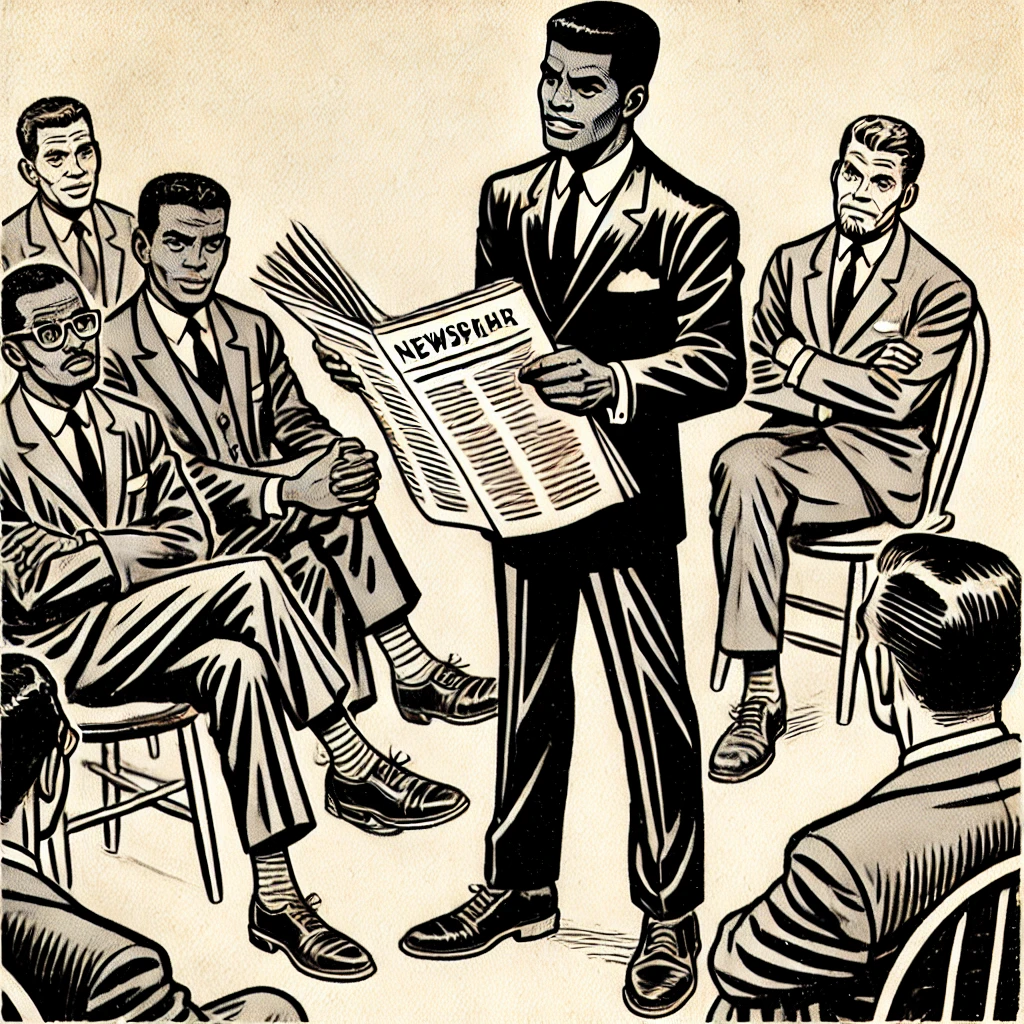
The Revelation: Breaking News in 1972
In July 1972, a significant turning point occurred concerning the Tuskegee Syphilis Study, as investigative journalism brought to light the unethical practices that had persisted for decades. The Associated Press published a revealing article that exposed the harsh realities faced by the hundreds of African American men involved in the study, many of whom were unaware of their syphilis diagnosis or the fact that they were being denied proper medical treatment. This groundbreaking revelation stirred public outrage and catalyzed discussions about ethical standards in medical research.
The lead-up to this exposure involved relentless inquiries by journalists and advocates, including the work of writer and activist David F. L. Johnson, who gathered insights and testimonies that outlined the inhumane treatment of the participants. The article unveiled not just the study’s details, but also the profound consequences it posed to those affected, ultimately revealing a breach of ethical guidelines that prioritize patient welfare. The public’s reaction was one of disbelief, as many could not fathom that such an egregious violation of trust had been tolerated for so long within a respected medical institution.
This public disclosure had far-reaching implications in the field of medical ethics. It prompted the establishment of stricter regulations concerning informed consent and overall patient rights in research settings. The fallout from the Tuskegee Syphilis Study reshaped the relationship between health institutions and the communities they serve, highlighting the crucial need for transparency and ethical accountability. Public trust, once shaken, compelled many to re-evaluate how medical research was conducted, ensuring that the tragic lessons of the past would not be forgotten.
Impact and Consequences of the Tuskegee Syphilis Study
The Tuskegee Syphilis Study, which took place from 1932 to 1972, profoundly impacted both the individuals directly involved and the broader community within which they resided. The study’s unethical nature led to devastating psychological consequences for the participants, who were misled about their health status and treatment. Many individuals experienced profound feelings of betrayal and mistrust towards the medical establishment, as they had been subjected to a prolonged process of observation without informed consent. This breach of ethics not only affected the participants but also reverberated through their families, instilling a legacy of mistrust that influenced health-seeking behaviors among African Americans for generations.
Beyond the immediate effects on individuals, the Tuskegee Study significantly shaped the landscape of medical ethics and public health policy in the United States. The public outcry following the study’s revelation in the 1970s prompted critical discussions around informed consent, patient rights, and the ethical obligations of researchers. This led to the establishment of stricter ethical guidelines for conducting research, most notably the Belmont Report, which delineates principles of respect for persons, beneficence, and justice.
The fallout from the Tuskegee Study also ignited conversations regarding racial relations and systemic inequities in healthcare. It underscored the need for a more equitable approach to medical treatment and research, prompting legislative measures such as the National Research Act of 1974. This Act aimed to protect human subjects in research, marking a significant shift towards accountability within medical institutions. The lingering effects of the Tuskegee Syphilis Study persist, making it a crucial case study for examining the intersection of ethics, race, and public health. As we reflect on this dark chapter in medical history, it becomes evident that addressing these historical wrongs remains critical to fostering trust and improving health outcomes in marginalized communities today.
Lessons Learned and the Path Forward
The Tuskegee Syphilis Study serves as a profound reminder of the ethical responsibilities that accompany medical research. This study, which spanned from 1932 to 1972, involved the exploitation of African American men who were misled about their health status. The study’s ethical violations led to widespread societal repercussions, highlighting the importance of ethics in medical investigations. A crucial takeaway from this dark chapter in American history is the necessity for informed consent. Participants must have a thorough understanding of their involvement in research, including potential risks and benefits, ensuring autonomy and respect for individual rights.
Moreover, ongoing concerns regarding racial disparities in healthcare underscore the need for ethical vigilance. African American communities, historically subjected to harmful medical practices, continue to face skepticism towards healthcare systems. This distrust can lead to reluctance in seeking necessary medical care, thus perpetuating adverse health outcomes. Addressing these disparities requires a commitment from healthcare professionals and researchers to implement transparency and accountability in medical practices. By fostering an environment of openness, individuals are more likely to feel secure in their interactions with healthcare providers, which is essential for improving health outcomes in marginalized communities.
Current efforts to strengthen relationships between healthcare providers and disenfranchised groups focus on community engagement and participatory research. Initiatives that prioritize the voices of marginalized populations contribute to rebuilding trust and establishing equitable healthcare practices. Additionally, implementing rigorous ethics training in medical education is vital for developing a new generation of healthcare professionals who value ethics as a core component of their practice. As we move forward, it is imperative that the lessons learned from the Tuskegee Syphilis Study guide our path, ensuring that history does not repeat itself and that ethical vigilance remains at the forefront of medical research.